ROR2 blockade as a therapy for osteoarthritis
In a new study, published in the journal Science Translational Medicine, researchers from Queen Mary University of London have developed a prototype drug that can heal cartilage and simultaneously help with pain. In this research Q&A Dr Anne-Sophie Thorup from the Centre for Experimental Medicine and Rheumatology explains why the findings are significant.
What is new about the study?
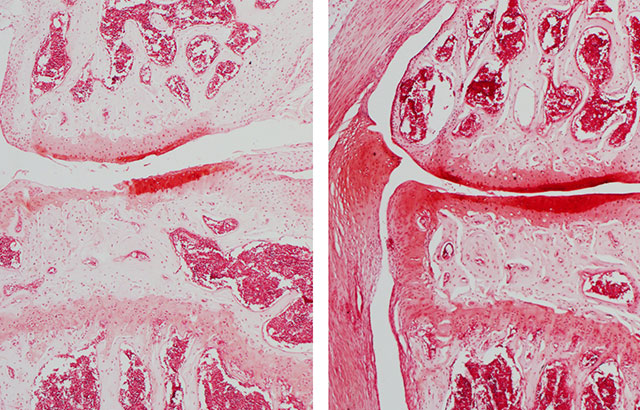
Throughout life we all develop lesions in the cartilage. For many people, especially after a certain age, cartilage loss becomes so bad that the bones grind against each other and that causes severe and disabling joint pain. Some patients lose their independence, cannot go shopping, cook and need help for basic tasks such as getting into and out of the bath. For these people there are currently only pain killers, but no drug is available to restore cartilage. At some point they need a joint replacement, which gives back some degree of independence, but it has a limited lifespan. We have developed a prototype drug that can heal cartilage and simultaneously help with pain. This is achieved by blocking a molecule called ROR2. We have opened the door for a medicine to treat osteoarthritis: the leading cause of disability worldwide. With some modifications, this approach can be used in patients.
How did you carry out the study?
This study was carried out mainly in mice. We could see that blocking ROR2 in mice with osteoarthritis helped the cartilage and also improved pain. We also showed that blocking ROR2 encouraged human cartilage cells to form new cartilage. Therefore we have a good indication that the same approach will work in patients, not only in mice.
Is there anything surprising about the results?
Yes, not only did blocking ROR2 improve the cartilage, but it also provided rapid pain relief, well before this effect could be explained by the restoration of the cartilage. This is important because if patients had to wait for years before experiencing pain relief, they would certainly stop taking the medication, particularly if it comes as an injection into the joint. We believe that the pain relief is independent of the protective effect of cartilage and it will make an enormous difference for the patients.
Why is the study important?
This study is important for two main reasons. Firstly, there is a good chance that it will radically transform the management of patients with osteoarthritis: currently there is very little that we can do for them until their joints are completely destroyed and are ready for replacement. We expect that in the future patients with osteoarthritis will just need to take the medication and will return to their active lifestyle and avoid surgery. We want to turn osteoarthritis care from being essentially surgical to a medical one.
What are the wider implications?
Currently osteoarthritis is the first cause of absenteeism in the UK and one of the top causes of disability worldwide. To give a sense of the size of the problem, including the loss of work days, the need for care, and indirect costs osteoarthritis accounts for a staggering 1.5-2% of the GDP in western countries. Therefore, returning these patients to their active life will have huge economical and societal consequences.
This research was conducted in Professor Francesco Dell'Accio's lab and funded by the Medical College of St Bartholomew's Hospital Trust, the William Harvey Research Foundation and FOREUM.
Further information
- Research paper: 'ROR2 blockade as a therapy for osteoarthritis' by Thorup et al. Science Translational Medicine. DOI: 10.1126/scitranslmed.aax3063
- Find out more about the Centre for Experimental Medicine and Rheumatology