Multiple Endocrine Neoplasia type 1 (MEN1)
View other pituitary disorders
MEN1 is an inherited disorder that causes tumours in various endocrine glands. MEN1 is sometimes called multiple endocrine adenomatosis or Wermer's syndrome, after one of the first doctors to recognise and describe it. MEN1 is rare, occurring in about one in 30,000 people. The disorder affects both sexes equally and shows no geographical, racial, or ethnic preferences.
Endocrine glands release hormones into the bloodstream. Hormones are powerful chemicals that travel through the blood, controlling and instructing the functions of various organs. Normally, the hormones released by endocrine glands are carefully balanced to meet the body's needs.
In patients with MEN1, several endocrine glands form tumours and become hormonally overactive. This is an important distinction from patients with FIPA, where no other endocrine glands form tumours. in MEN1 the overactive glands most often include the parathyroid glands, the pancreas and the pituitary. Most people who develop excessive hormonal production from only one endocrine gland do not have MEN1.
The Parathyroid Glands
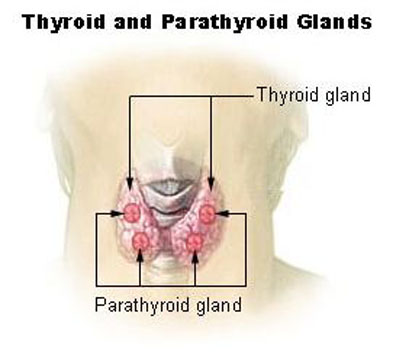
The parathyroids are the endocrine glands earliest and most often affected by MEN1. The body normally has four parathyroid glands, which are located close to the thyroid gland in the front of the neck. The parathyroids release into the bloodstream a chemical called parathyroid hormone (PTH), which helps maintain a normal supply of calcium in the blood, bones, and urine.
Hyperparathyroidism
In MEN1 patients, all four parathyroid glands tend to be overactive, causing hyperparathyroidism. The parathyroid glands form tumours that release too much PTH, leading to excess calcium in the blood. High blood calcium, known as hypercalcaemia, can exist for many years before it is found due to symptoms or by accident or through screening for MEN1. Hypercalcaemia can cause excess calcium to spill into the urine, leading to kidney stones or kidney damage. Also, the bones may lose calcium and weaken leading to osteoporosis.
Nearly everyone who inherits a susceptibility to MEN1 will develop hyperparathyroidism by age 50, but the disorder can often be detected before age 20. Hyperparathyroidism may cause no problems for many years, or it may cause tiredness, weakness, muscle or bone pain, constipation, indigestion, kidney stones, or thinning of bones.
Doctors must decide whether hyperparathyroidism in MEN1 is severe enough to need treatment, especially in a person who has no symptoms. The usual treatment is an operation to remove most or all of the parathyroid glands. One option is to remove the three largest glands and all but a small part of the fourth. Another is to remove all four glands and at the same time transplant a small part of one gland into the forearm. By maintaining a portion of one gland, the parathyroid transplant continues to release PTH into the bloodstream to do its job.
After parathyroid surgery, regular monitoring of blood calcium is needed because often the small piece of remaining parathyroid tissue grows larger and causes recurrent hyperparathyroidism. If the remaining piece is in the forearm and additional surgery is needed to remove more parathyroid tissue, the arm operation can be performed under local anaesthesia.
Sometimes all four glands are completely removed to prevent recurrence or may be unintentionally removed during parathyroid surgery. People whose parathyroid glands have been completely removed must take daily supplements of calcium and vitamin D or another related treatment to prevent hypocalcaemia, or low blood calcium.
The Pancreas and Duodenum
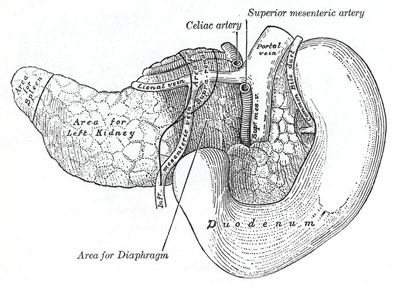
Located behind the stomach, the pancreas has two major roles:
- To release digestive juices into the intestines and
- To release key hormones into the bloodstream.
The duodenum is the first part of the small intestine next to the pancreas. The pancreatic hormones are normally produced by small clusters of specialized cells called pancreatic islets. Some of the major hormones produced by the pancreatic islets are
- Insulin - lowers blood glucose
- Glucagon - raises blood glucose
- Somatostatin - inhibits secretion of certain other hormones especially growth hormone
- Vasoactive intestinal peptide (VIP) - causes intestinal cells to secrete water into the intestine
- Gastrin - causes the stomach to produce acid for digestion
Gastrinomas
In MEN1 patients, gastrin may be oversecreted by tumours called gastrinomas in the pancreas or the duodenum. If exposed to too much gastrin, the stomach releases excess acid, leading to the formation of severe ulcers in the stomach and small intestine. In addition, too much gastrin usually causes serious diarrhoea.
People with MEN1 have about a 20 to 60 percent chance of developing gastrinomas. The collection of symptoms associated with gastrinomas is called Zollinger-Ellison syndrome. The ulcers caused by untreated gastrinomas are much more dangerous than typical stomach or intestinal ulcers. Left untreated, they can cause rupture of the stomach or intestine and even death.
The gastrinomas associated with MEN1 are not easily cured through tumour removal at surgery as often several small gastrinomas can be found in the pancreas, duodenum, and lymph glands. The mainstay of treatment is powerful medicines called acid pump inhibitors that block stomach acid release. Taken by mouth, these medicines have proven effective in controlling the complications of excess gastrin in most cases of Zollinger-Ellison syndrome. Treatment with somatostatin analogues is also used.
Occasionally, a person who has MEN1 develops another islet tumour of the pancreas that secretes high levels of hormones. Insulinomas, for example, produce too much insulin, causing hypoglycaemia, or low blood glucose. About 10 percent of adults with MEN1 develop insulinomas. Rare pancreatic tumours may secrete too much glucagon, which can cause diabetes, or too much VIP, which can cause watery diarrhoea. In general, surgery is the mainstay of treatment for these uncommon types of tumours.
The Pituitary Gland

The pituitary, a small gland located at the base of the brain, produces many important hormones that regulate basic body functions. For further details on the pituitary gland click here. The normal major pituitary hormones are
- Prolactin - controls the formation of breast milk and influences fertility and bone strength
- Growth hormone - regulates body growth, especially during adolescence
- ACTH - stimulates the adrenal glands to produce cortisol
- TSH - stimulates the thyroid gland to produce thyroid hormones, which regulate metabolism
- Luteinizing hormone and FSH - stimulates the ovaries or testes to produce sex hormones and to produce eggs and sperm
Prolactinomas
The pituitary gland develops a tumour in about one in four people with MEN1. This tumour most often releases too much prolactin, called a prolactinoma. High prolactin levels can cause excessive production of breast milk or interfere with fertility in women or with sex drive and fertility in men.
Treatment may not be needed for prolactinomas. If treatment is needed, medicines known as a dopamine agonists (bromocriptine, cabergoline) can effectively shrink the tumour and lower the production of prolactin. Occasionally, prolactinomas do not respond well to this medication. In such cases, surgery, radiation, or both may be needed.
Other pituitary tumour types in MEN1 can ne non-functioning pituitary adenoma (NFPA) or growth hormone-sereting adenoma.
Further reading on MEN1 can be found at the following websites:
- AMEND http://www.amend.org.uk
- ENEA http://www.eneassoc.org